IVF in the world of IP
Katie Goulding, Senior Associate and Chartered Trade Mark Attorney at CMS, now mum of two, shares her experience of IVF treatment in the hope of reducing the number of women going through IVF without workplace support.

NOTE: The following piece discusses infertility, IVF treatment and loss. If you are experiencing any of these things, know that it is okay not to read it.
It isn’t easy putting our experience of infertility on paper. I’ve tried more than once but have put it aside for failing to get across in words the enormity of the impact of it but I’m going to give it a go.
Infertility is a personal experience - there are shared aspects, sometimes common thoughts and emotions – but, ultimately, no two experiences are likely to be exactly the same.
So, this is my own (very) personal account. I couldn’t write about it any other way.
While the challenges that we faced were exhausting and overwhelming, IVF brings different hurdles to different people.
For example, Black and minority ethnic women are likely to see worse outcomes from IVF, due in part to racial inequalities in healthcare. Therefore, undergoing IVF comes with higher risks and more rounds may be needed to conceive.
Additionally, female same-sex couples must undergo between six and 12 rounds of IUI (Intrauterine Insemination) before becoming eligible for NHS funded IVF. IUI typically costs around £1000 per round, representing a substantial additional financial burden.
One thing that is common is that most of us who do decide we want to procreate one day, simply take it as a given that we will. My husband and I were going to have kids.
No what ifs, buts, heavy conversation or debate, it was just a fact we agreed on very early in our relationship and the only question to be answered was “when?”.
Our friends had kids. We were “the best auntie and uncle”, so we were going to be great parents. It just wasn’t in our contemplation that we might not.
We did not foresee nearly five years of devastation. That isn’t hyperbolic. Infertility, whether treatment is successful or not, is devastating. A profound grief for something you never had - and we are living it while managing workloads and deadlines and politics and everything else life throws at us.
Forward planning

On 22nd May 2018, after another beautifully sunny day in Seattle, I packed my suitcase. It was my last full day of INTA 2018, a major conference for trade mark legal professionals like myself.
I’d put a couple of hours aside and planned to venture out and pick up some gifts for home - what I hadn’t planned is for my period to start.
“My God, why is she talking about her period?!” Well, because of my period, that day became day one of our first IVF (ICSI) treatment.
My period came early, unpredictably so. Timings are crucial in IVF treatment. Scans, hormone injections, blood tests, are all meticulously plotted.
The instructions from our clinic were simple: as soon as period arrives, phone the clinic so that baseline bloods and a scan can be carried out at day two.
The results of those two things inform parts of the protocol. Except I wasn’t due to arrive back in the UK until 24th May (day four) and I couldn’t call the clinic because I was -eight hours and clinic was closed. Panic.
Were speed limits broken between Manchester Airport and Jessops Clinic Sheffield on 24th May? I plead the Fifth. By then, we had been trying to conceive (“Trying to conceive” is often abbreviated by medical professionals to TTC) for more than three years.
IVF and the IP profession
Am I trying to force a link between fertility and the IP profession with a tenuous reference to INTA? No - I don’t have to. Because there already is one.
More than 50,000 undergo IVF treatment annually, but more than half of women (58%) do not feel able to tell their employer.
With 60% of CITMA members being women, it is evident that this issue is particularly prevalent within our community.
Additionally, those statistics just speak of those undergoing treatment. If so few women are telling employers that they are undergoing treatment, imagine how few are telling their employers they are trying to conceive.
To further inclusivity and support within our profession we need to talk about it.
There is a silent suffering in infertility long before (and after) colleagues become aware that someone is going through it at all.
How much easier would it be if workplace support was signposted – the same way we flag maternity policies and annual leave policies and the rest of it?
If frameworks were put in place so that those trying to conceive could be assured by defined “processes” and collective experience.
Periods and new baby announcements
Sorry (not sorry) to talk about periods again but, to state the obvious, women trying to conceive (TTC) are not always in the safety of their home when their period arrives.
That means there is a good chance, at some point, that a woman you work with has
nipped to the loo and had their heart break there. Time and time again, month after month.
But we’re not talking about it. So, what happens? I’ll tell you what I did (the same thing I did when another email announcement with photo of beautiful baby landed in my inbox or another collection crossed my desk – pregnant women and babies are everywhere when trying to conceive).
I stood up, walked out of the building, and ran to my parked car to come undone. Wipe away the tears, straighten up, return to the office, carry on. Carry on. Because it’s not easy to explain it when no one is talking about it. We need to talk about it.
I could tell you that I was still happy for them, pregnant friends and colleagues, that I could put aside what we were going through and feel happiness for those around me but, honestly, for the most part, that isn’t exactly the truth of it.
It hurt too much, and I envied them too much. I know from speaking to others, it’s common to beat yourself up about this. Don’t! There isn’t the headspace for it.
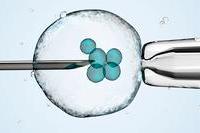
The medical process
As if the emotional thrashing isn’t exhausting enough, the women around us who have started a treatment cycle then have their hormones manipulated with typically (and in the case of ‘suppression’ at stage 1) at least 24 injections before egg retrieval, including follicle stimulating injections for 9-12 days and a HCG hormone injection three days prior to egg retrieval to help eggs mature (and that isn’t counting all the investigations that have been carried out leading up to treatment itself).
After that it’s the pessaries and I’ll spare you any more detail on those little (not at all little)… things. At least three to five (transvaginal) scans, possibly more bloods… you get the picture.
If you want to create a culture where these things can be talked about or at least better understood, I implore you, at the very least, to read more about the procedure and make resources accessible via your intranet pages.
Treatments can vary by clinic and, obviously, patient to patient but the main steps of a typical treatment can be found on the NHS website.
Side effects at work
Side effects? Of course. Again, they vary in degree and type by individual but you should expect that your colleague is suffering one or more of these: nausea, vomiting, headaches, (uncontrollable) fluctuating moods, injection site swelling, rashes, tenderness, bleeding and, at the more severe end, hyperstimulation of the ovaries (OHSS) which can be dangerous for patient and also mean treatment being paused.
The only person who knows if they can / should continue working when enduring the emotional and physical thrashing of IVF is the patient.
For some, work is a welcome distraction. It often was for me.
However, not taking time away from work and continuing to work at the same pace or capacity are not the same thing.
I feel strongly that it is someone else’s responsibility to remove the workload pressures and to handle the temporary redistribution of work, be that a manager, HR or other designated person.
I emphasise the word temporary because the last thing an individual dealing with infertility/treatment should have to worry about is the loss of work and opportunity when they return.
The two weeks wait

The two weeks wait for results day is the worst part.
At embryo transfer the sonographer said to us “watch the screen, watch for the little star”. Our embryo. I loved that little star.
I cannot tell you how hard it is to get through those days trying not to dare to imagine the person that star might be. Trying not to test. Trying to think of anything other than results day. It feels like a lifetime.
Colleagues may prefer to work through this time to try to pass it. Appearances can be deceiving.
They need your flexibility and support now possibly more than ever, as an unsuccessful outcome is a real possibility.
Allow your colleagues the time and space to grieve. It is a loss, different to other losses but a loss nonetheless.
Infertility. Shall we have a chat about it?
How you can help
Move baby/child announcements to a dedicated place on internal intranets. Allow vulnerable colleagues to consume this news when and if they choose.
- Educate yourself and colleagues. Treatments can vary by clinic and, obviously, patient to patient but the main steps of a typical treatment can be found on the NHS website. Make resources easily accessible on company intranets.
- Clearly set out your values around fertility and develop a policy so that you can provide the support that is needed. Fertility Network UK is just one of many offering fantastic initiatives to help employers develop fertility policies.
- Create an affinity group dedicated to fertility and adoption.
- Don’t try to be a fertility advisor. No amount of herbal tea, acupuncture or walks are going to miraculously undo a “diagnosis” of infertility.
- Encourage client “teams” and workflows that are equipped to deal proactively and reactively to a colleague being away, at short notice or otherwise. Move those watch notices!
- Help colleagues temporarily off-load additional projects and workstreams and carry out regular check-ins to facilitate the return of those things when your colleague is ready.
- Have a safe closed-door space for colleagues to escape.
- Your colleague does not want to know that you had a friend who conceived when they “relaxed” or “stopped trying”.
- Don’t whinge (too much) about your kids to colleagues TTC. It’s a hard one. We all do it and we absolutely should talk freely about the challenges of parenting. Simply be mindful of when and how often you do it with a vulnerable colleague.
- Know the law and then do better than it! There is currently no statutory right for time off for pre-conception care or fertility treatment. The Fertility Treatment (Employment Rights) Bill which would require employees a right to paid medical leave for fertility treatment, has had its second reading. You can read more here.
- Talk about it.


